3 month trach change out
- jjj0urney
- Nov 8, 2017
- 3 min read
Jason's trach gets changed out every 3 months and was done on Wednesday, November 8. I'm not sure I've explained why this procedure is done every 3 months though. Trach products are made for short term use. If you've ever been in or had a family member in an emergency situation, an airway is gained from the mouth and the person is unconscious and restrained (so they don't pull at the airway in the mouth). A trach through the neck is for a longer situation, where a person is improving enough to be awake but the lungs aren't healed yet. Well, in the ALS world, the lungs will not heal, so the trach becomes a permanent situation. Unfortunately, trach products have never been developed that last that long. We (as well as most of the US) use Shiley products and written in the instructions for use, it specifically says "manufacturer recommends that the Tracheostomy Tube usage not exceed 29 days." The plastic and the balloon do wear over time and it is just good to check in. Protocol for ALS patients at Emory is to change out the device every 3 or so months. Side note: different doctors disagree on this-some say it is OK to wait 6 months or wait until there are issues...
As it was placed at the beginning of May, change out was due in August and was done while in the hospital with pneumonia. Orders were simply to get the device changed out and it went easy and well right there in the ICU room. This was our second time getting changed out, but they did a little more than back in August. Our main campus Emory doctors say they like to do a broncoscopy with trach change just to make sure nothing new is going on and no trauma has happened. They like to get a full picture, I should say.
After some difficulty placing an IV for some conscious sedation (pulling the device out and placing back in the neck is uncomfortable!), we were off to the OR. Here is something I've learned with ALS patients and their family: doctors would much rather have me in the room than not, even if it means I go into the OR. I was in the OR during the entire procedure as the broncoscopy was being done. Dr. Berkowitz and Brittany (nurse practitioner) did not like what they saw in the lungs. The mucous was thick, abundant, and discolored.
They ordered a 10 day antibiotic for us to pick up on the way home. A large sample was sent off for culture. They also did a chest xray (with no significant issues) before we left. Jason did not feel well on his birthday (November 9) and we decided to watch a movie at home instead of our planned theater trip, but temperature only got to 99.6. On Friday, Nov 10, the sample came back with >100K Strep Constellatus (part of the Strep Anginosus group) and no susceptibilities had grown yet. We were told to continue the antibiotic and if he had a fever or did not feel better, prepare for admission for IV antibiotics. What this means is that bacteria grew in a petri dish from the sample. It also means that antibiotics were put on the bacteria to try and kill it and so far, all the antibiotics were working. If over the weekend, an antibiotic proves to not work on the bacteria, it is not recommended to use. The doctors would change it if it did not kill the bacteria in the petri dish (called susceptibility). On Tuesday, Nov 14, the cultures were complete and showed the antibiotic Jason was taking was OK to complete and did not need to be changed, which is great! Antibiotics have their own side effects.
Another thing that we brought up pre OR was the fact that the trach leaks. The doctors explained that this is because of a buildup of mucous above the cuff from swallowing and such...just in case this helps-picture below!
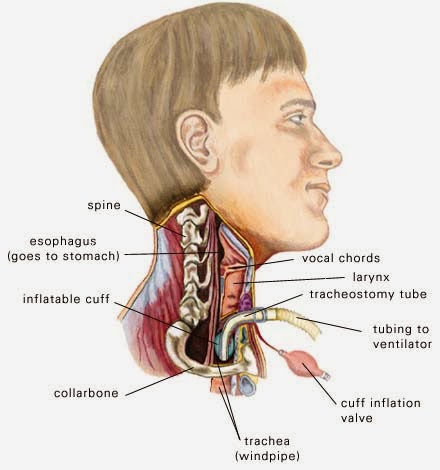
They have encouraged us to deflate the cuff so that the secretions can go into the lungs (the vent will blow some up and out of the mouth as well) then suction it out to get rid of it. This also does so many other things, like prevent infection, prevent skin breakdown inside and outside of the neck, and keep us from having to constantly add air to the cuff to hold the fluid. We have honestly always thought deflation of the cuff was optional, not necessarily encouraged, so you learn something new everyday! Problems with a permanent trach that are just not google-able!






Comments